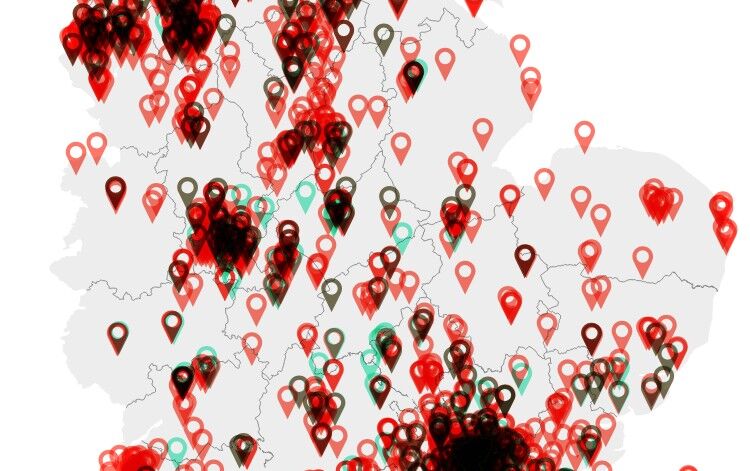
EXCLUSIVE: The Pharmacist mapped community pharmacy closures across England over the last five years, and uncovered a net loss of more than 1,000 bricks and mortar pharmacies since 2019.
Read the first article in our series on how pharmaceutical services are changing in England:
Of the 11,893 community pharmacies registered with the General Pharmaceutical Council (GPhC) in March 2019, just 10,260 remained in April 2024 – suggesting a total of 1,633 closures over five years.
In the same time period, 410 new community pharmacies opened – just one for every four that had closed – indicating a net loss of 1,223 pharmacies over the five years.
While the GPhC data includes pharmacies providing both private and NHS pharmaceutical services, analysis of the NHS England Pharmaceutical List indicates that 90% of those pharmacies lost were providing NHS community pharmacy services.
Related Article: What could Kinnock's vision for pharmacy 'reform' look like?
Figures provided by the NHS Business Services Authority indicate a net loss of 1,102 non-distance-selling community pharmacies in the same time period.
Vicki Roberts, chief executive officer of Community Pharmacy South Yorkshire, told The Pharmacist that in her opinion, the ‘unacceptable rate’ of closures was ‘jeopardising access to pharmaceutical services for some patients’.
‘NHS England has a duty to ensure that the population has adequate access to pharmaceutical service provision,’ she said, but described this as currently ‘questionable’.
She added that for many patients, pharmacy closures would lead to ‘difficulties accessing their medicines, clinical services and general healthcare’.
And for pharmacies that remained open, local closures often meant they were ‘having to make difficult business decisions such as suspending advanced service provision while they struggle to cope with the increased prescription volume’.
‘All readers will be familiar with the term “dispensing at a loss” and therefore increasing prescription volume is not necessarily a positive for contractors,’ she added.
‘There are many contributing factors to this situation but most notably a community pharmacy contractual framework and flat funding model that is not fit for purpose.
‘The funding model that pharmacy contractors currently work to takes no account of inflation or dispensing volume increases – both of these are huge flaws in their own right but together make for an untenable situation for many pharmacy contractors,’ Ms Roberts suggested.
And other pressures such as workforce issues and rising costs also played a part, she said.
She noted that the recruitment of pharmacists and pharmacy technicians into NHS-funded Additional Roles Reimbursement Scheme roles in general practice ‘continues to be a challenge’.
Related Article: Beyond ARRS: The impact and future for community pharmacy
Meanwhile, an increasing number of contractors were also struggling to recruit dispensers and healthcare assistants as they were ‘unable to offer attractive rates of pay and simultaneously keep their businesses viable’.
‘Pharmacy closures impact everyone, most notably the pharmacists and staff that work within them and patients but also local GP practices, other pharmacies and other nearby retail premises,’ Ms Roberts said.
‘Often a community pharmacy is the heart of a community, providing much more than somewhere for a local resident to collect their prescription from which, following closure, may leave a neighbourhood without an easily accessible health and care port of call.’
Janet Morrison, chief executive of Community Pharmacy England, said the analysis showed ‘the stark reality of the situation’.
‘Community pharmacies are in deep distress, with many on the brink of collapse,’ she said, noting similar findings from CPE’s 2024 Pharmacy Pressures Survey.
Ms Morrison added: ‘Permanently closing is an absolute last resort for pharmacy owners, with any closure having a detrimental impact on patients as well as increasing the pressure on other pharmacies.
‘The accelerating reduction in pharmacies in recent years is testament to the crippling effect that the relentless financial and operational pressures on community pharmacy are having.’
Related Article: Pharmacy First: A year of the service in England
And she said that ‘the viability of all pharmacy businesses’ was the negotiator’s ‘critical concern in funding discussions with policymakers’.
‘It is imperative that the government and the NHS increase both the funding and support available for community pharmacies, and put them on a sustainable footing,’ she told The Pharmacist.
This is the first article in our series on how pharmaceutical services are changing in England.

Have your say
Please add your comment in the box below. You can include links, but HTML is not permitted. Please note that comments are not moderated before publication and the views expressed are those of the user and do not reflect the views of The Pharmacist. Remember that submission of comments is governed by our Terms and Conditions. You can also read our full guidelines on article comments here – but please be aware that you are legally liable for any libellous or offensive comments that you make. If you have a complaint about a comment or are concerned that a comment breaches our terms and conditions, please use the ‘Report this comment’ function to alert our web team.